Most Common Medical Malpractice Claims in Minnesota (2025) highlight how the legal system helps protect patients and improve healthcare standards. By recognizing common claim types such as delayed diagnosis or surgical mistakes, Minnesotans can better understand their rights and feel empowered to ask the right questions about their care.
Medical malpractice claims aren’t about blame; they are about accountability, safety, and learning from mistakes to prevent future harm. If you have experienced unexpected outcomes in treatment, exploring the most common medical malpractice claims in Minnesota can provide clarity, reassurance, and the opportunity to move forward with trusted legal guidance.
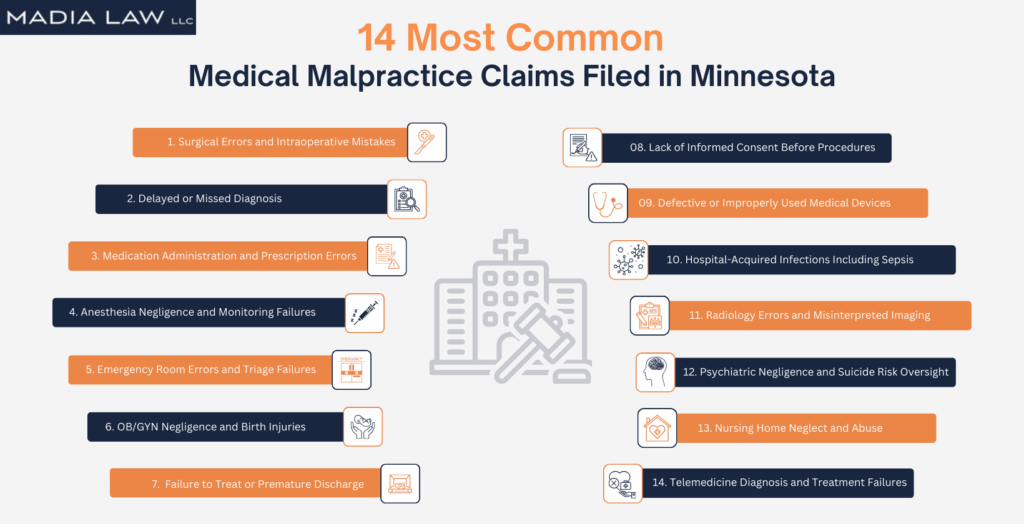
14 Most Common Medical Malpractice Claims Filed in Minnesota
Not every bad medical outcome is malpractice — but when a provider’s mistake leads to preventable harm, the law may recognize it as negligence. The following are 14 of the most common medical malpractice claims filed in Minnesota, based on real cases where patients suffered serious injury due to substandard care.
By understanding these common patterns, patients and families can better identify when a medical error may have crossed the legal threshold — and take the first step toward holding providers accountable.
1. Surgical Errors and Intraoperative Mistakes
Surgical errors are among the most serious and preventable forms of medical malpractice. These mistakes occur when a surgeon, nurse, or surgical staff member deviates from the accepted standard of care, causing direct harm to the patient.
In Minnesota, surgical malpractice lawsuits often stem from clear breaches of protocol, such as:
- Performing the wrong procedure or operating on the wrong body part
- Leaving instruments, sponges, or other foreign objects inside the patient
- Causing unintended damage to nearby organs, nerves, or tissues
High-risk specialties, such as orthopedics, cardiovascular surgery, and neurosurgery, face a higher incidence of malpractice claims due to the complexity of procedures and the precision required. When surgical negligence leads to preventable harm, pursuing legal action not only helps victims recover compensation, but it also promotes safer practices for future patients.
2. Delayed or Missed Diagnosis
When a diagnosis is delayed, or missed entirely, the consequences can be life-altering. In high-stakes conditions like cancer, stroke, or internal infections, even a small delay can mean the difference between recovery and irreversible harm.
Under Minnesota law, medical malpractice occurs when a healthcare provider fails to diagnose a condition that a reasonably competent professional would have identified, resulting in avoidable injury or worsened prognosis.
Some common scenarios include:
- Failing to detect cancer until it has progressed to an advanced, less treatable stage
- Misreading or ignoring stroke symptoms during emergency evaluation
- Overlooking early warning signs of sepsis, internal bleeding, or post-surgical infections
Several high-profile Minnesota cases have shown how delayed diagnoses, especially involving cancer can lead to significantly shortened life expectancy, aggressive treatment plans, and emotional trauma for families. To pursue a delayed diagnosis claim, it must be shown that an earlier diagnosis was not only possible but would have meaningfully changed the outcome.
3. Medication Administration and Prescription Errors
Medication errors are a leading cause of preventable harm in healthcare, and they can occur at any stage, from prescribing and dispensing to administering the wrong drug or incorrect dosage. These mistakes often stem from communication breakdowns, inaccurate charting, or failure to check for drug interactions and known allergies.
Common consequences include:
- Overdoses caused by dosage miscalculations
- Severe allergic reactions from overlooked contraindications
- Dangerous drug interactions leading to seizures, organ failure, or even death
Depending on where the error occurred, liability may rest with physicians, pharmacists, nurses, hospitals, or nursing homes. High-risk medications, such as insulin, opioids, and blood thinners, are especially prone to catastrophic outcomes when mishandled. When patients suffer harm from preventable drug errors, legal action plays a vital role in securing compensation and driving accountability across the healthcare system.
4. Anesthesia Negligence and Monitoring Failures
Anesthesia errors are among the most dangerous types of medical malpractice, as even minor mistakes can cause severe, lifelong harm. Anesthesia negligence typically involves improper dosing, failure to monitor vital signs, or neglecting a patient’s medical history—all of which can lead to serious complications during surgery.
Common anesthesia-related failures include:
- Administering too much or too little anesthesia
- Failing to monitor oxygen levels, blood pressure, or heart rate
- Overlooking medication allergies or preexisting health conditions
- Delayed response to complications or equipment malfunctions
When vital signs are not properly monitored or red flags are missed, patients can suffer brain damage, nerve injuries, or even death. Both anesthesiologists and surgical teams may be held legally responsible if they fail to follow established safety protocols. These cases often reveal how proper vigilance and communication could have prevented devastating outcomes.
5. Emergency Room Errors and Triage Failures
Emergency rooms are high-pressure environments—but when rushed decisions or poor triage protocols lead to preventable harm, it can be considered malpractice. ER negligence occurs when staff fail to recognize life-threatening conditions, delay urgent care, or discharge patients before they’re medically stable.
Examples of emergency room malpractice include:
- Misdiagnosing a heart attack or stroke as anxiety or indigestion
- Delayed treatment of sepsis, resulting in organ failure
- Discharging a patient without reviewing critical lab results
- Overlooking internal injuries during overcrowded shifts
In busy Minnesota hospitals, these breakdowns in care can cost patients valuable treatment time, and in some cases, their lives. Prompt diagnosis and swift intervention are critical in emergency care. When hospitals fail to meet that standard, victims and families deserve answers and accountability.
6. OB/GYN Negligence and Birth Injuries
Mistakes during pregnancy, labor, or delivery can have devastating and lifelong consequences for both mother and child. OB/GYN negligence occurs when a healthcare provider fails to meet the accepted standard of care, resulting in serious complications that are often preventable with timely intervention and proper monitoring.
Common examples of obstetric malpractice include:
- Failing to perform an emergency C-section when signs of fetal distress
- Misusing forceps or vacuum devices during delivery
- Overlooking signs of maternal hemorrhage, infection, or preeclampsia
- Delayed response to umbilical cord prolapse or fetal oxygen deprivation
In many cases, conditions like cerebral palsy or brachial plexus injuries could have been avoided with more attentive care. These birth injury cases require in-depth legal investigation to determine whether malpractice occurred and which members of the medical team may be held liable. Families deserve both answers and justice when negligence disrupts the start of a new life.
7. Failure to Treat or Premature Discharge
When a patient is discharged too soon, or their symptoms are ignored altogether, the results can be catastrophic. This form of medical malpractice often occurs when providers downplay clear warning signs, underestimate the seriousness of a condition, or fail to arrange proper follow-up care. Under Minnesota law, healthcare professionals have a legal duty to treat patients in line with the accepted standard of care—including ensuring that discharge decisions are safe and medically justified.
Premature discharge and failure-to-treat cases frequently involve:
- Post-operative infections that worsen without monitoring
- Unstable vital signs or unresolved cardiac symptoms
- Internal bleeding or undiagnosed surgical complications
- Respiratory conditions such as pneumonia or shortness of breath
- Severe dehydration, malnutrition, or neglect in vulnerable patients
- Psychiatric emergencies where suicide risk is ignored
Too often, these oversights occur in understaffed or high-turnover facilities, where miscommunication and rushed decision-making usually replace careful evaluation. When hospitals or providers cut corners, patients and their families are left to face avoidable harm, and may be entitled to legal action.
8. Lack of Informed Consent Before Procedures
Every patient has the right to make informed decisions about their medical care. Minnesota law clearly states that healthcare providers are legally and ethically required to clearly and understandably explain the nature of a procedure, its risks, benefits, and any reasonable alternatives before proceeding with treatment.
Informed consent is not just a formality—it is a foundational principle of patient autonomy and safety.
Common violations of informed consent include:
- Glossing over or skipping the discussion of serious risks
- Failing to present alternative treatment options
- Using complex medical jargon instead of plain language
- Performing procedures on minors without guardian approval
- Proceeding without interpreter services for non-English-speaking patients
When providers bypass consent protocols, they not only violate the law, but also put patients at unnecessary risk. Legal action may be appropriate if a procedure causes harm and the patient was not adequately informed.
9. Defective or Improperly Used Medical Devices
Medical devices play a critical role in diagnosing and treating serious conditions, but when these tools fail, the consequences can be life-threatening. A medical malpractice or product liability claim may arise when a device is inherently defective or improperly used by a healthcare provider. Patients can suffer serious harm if the device malfunctions, is used incorrectly, or is implanted without proper evaluation.
Commonly involved devices include hip replacements, pacemakers, insulin pumps, and surgical mesh. Liability can fall on physicians or hospitals for misuse, or on manufacturers for design flaws or inadequate instructions.
Device-related malpractice and injury claims often involve:
- Defective designs that cause breakage, malfunction, or early failure
- Manufacturing errors during production or sterilization
- Insufficient warning labels or misleading instructions for use
- Inappropriate device selection given the patient’s medical history
- Failure to monitor the device’s function after implantation
These cases require an in-depth investigation to determine whether the injury resulted from medical negligence, a product defect, or both.
10. Hospital-Acquired Infections Including Sepsis
Hospital-acquired infections (HAIs) are dangerous complications that develop during a patient’s hospital stay—often due to lapses in hygiene, sterilization, or infection control. These infections are not part of the patient’s original condition and are largely preventable with proper care and hygiene. Failure to follow basic safety protocols can result in severe, life-threatening complications.
In Minnesota, HAIs are a common source of hospital negligence claims, particularly when infections are linked to unsanitary equipment, poor post-operative care, or delayed diagnosis and treatment.
Common hospital-acquired infections include:
- MRSA (Methicillin-resistant Staphylococcus aureus)
- C. diff (Clostridioides difficile)
- Sepsis caused by untreated or undetected infections
- Surgical site infections following operations
- Urinary tract infections from improper catheter use
- Ventilator-associated pneumonia in ICU patients
11. Radiology Errors and Misinterpreted Imaging
Radiology plays a critical role in modern medicine; however, when providers fail to correctly interpret scans, delay reporting urgent findings, or neglect to share critical results with the treating team, it can be problematic. When radiology errors occur, patients often lose crucial treatment time, which can sometimes result in irreversible outcomes. These errors often lead to missed or delayed diagnoses of serious conditions such as cancer, aneurysms, or internal bleeding—conditions where early detection is essential for survival.
In high-volume hospitals, communication gaps between radiologists and other departments increase the risk of mistakes, making radiology errors a growing area of concern.
Common scenarios of radiology malpractice include:
- Failing to identify tumors in X-rays, CT scans, or mammograms
- Overlooking signs of brain hemorrhage or stroke in imaging studies
- Delayed reporting of urgent, life-threatening findings
- Not following up on abnormal or inconclusive imaging results
- Providing incomplete or inadequate documentation of radiology interpretations
12. Psychiatric Negligence and Suicide Risk Oversight
Mental health professionals have a critical duty to protect vulnerable patients by providing accurate diagnoses, prescribing safe and appropriate medications, and closely monitoring suicide risk. Ignoring warning signs, mismanaging treatment, or failing to intervene at the right time can have devastating consequences. These lapses are especially common in inpatient facilities or during medication changes, when patients are at their most vulnerable.
Families may have grounds for a legal claim if negligent psychiatric care results in suicide attempts, harm to others, or severe emotional decline.
Common forms of psychiatric negligence include:
- Failing to assess suicide risk during intake evaluations
- Prescribing improper medications or unsafe drug combinations
- Neglecting to monitor or supervise suicidal inpatients
- Dismissing patient history or ignoring concerns raised by family members
- Discharging a patient without a clear safety plan or follow-up care
13. Nursing Home Neglect and Abuse
Nursing home neglect occurs when long-term care facilities fail to provide residents with the basic standard of care required by federal nursing home regulations and Minnesota’s Vulnerable Adults Act. These failures often manifest as untreated bedsores, overmedication, dehydration, or preventable falls—and are sometimes concealed through staff cover-ups or left unreported due to fear of retaliation. Too often, it is family members who notice the warning signs long before a facility acknowledges the harm.
Residents of Minnesota nursing homes are protected under both state and federal law, and legal action may be appropriate when neglect results in injury, illness, or emotional trauma.
Common warning signs of nursing home neglect and abuse include:
- Pressure ulcers (bedsores) caused by inadequate mobility support
- Unexplained fractures or falls with no proper incident report
- Malnutrition or dehydration from missed meals or poor supervision
- Overmedication, chemical restraints, or sudden changes in prescriptions
- Poor hygiene, soiled bedding, or unsafe living conditions
- Emotional withdrawal, depression, or fear of certain staff members
14. Telemedicine Diagnosis and Treatment Failures
Telemedicine has transformed healthcare by expanding access to doctors and specialists, but it has also introduced new risks. Without the benefit of in-person examinations, providers may miss critical details, misinterpret symptoms, or overlook key aspects of a patient’s history. Technical glitches, rushed virtual visits, and poor follow-up protocols can further increase the risk of preventable harm.
These challenges became especially evident during the COVID-19 pandemic, when many patients relied heavily on digital platforms for care. Unfortunately, lapses in telehealth often result in delayed diagnoses, improper prescriptions, or confusion about treatment plans.
Common examples of telemedicine malpractice include:
- Failing to recognize stroke symptoms without proper neurological testing
- Missing red-flag symptoms during virtual visits, leading to delayed cancer diagnoses
- Overprescribing or causing dangerous drug interactions due to incomplete medication histories
- Missing follow-ups or mishandling scheduling on telehealth platforms
- Providing inadequate explanations of treatment plans, resulting in patient misuse or error
When virtual care falls below the accepted standard, patients may experience the same life-altering consequences as in traditional malpractice cases. Legal action can help ensure accountability and improve safety standards as telemedicine continues to grow.
For a legal consultation, call 612-349-2729
Why These Medical Errors Lead to the Most Lawsuits
The types of errors outlined above consistently lead to malpractice lawsuits because they involve clear breaches of the medical standard of care, cause significant and often irreversible harm, and are usually preventable with proper attention, communication, and adherence to established protocols. Unlike less severe mistakes, these failures strike at the heart of patient safety—surgery, diagnosis, emergency response, and ongoing care—where lives and long-term health outcomes are directly at stake.
Patients and families are also more likely to pursue legal action when:
- The harm is severe and life-changing, such as permanent disability, brain injury, or wrongful death.
- The error was avoidable, meaning another reasonably skilled provider would have acted differently and prevented the outcome.
- Trust was broken, as in cases of concealed infections, ignored warning signs, or procedures performed without proper consent.
- Costs are overwhelming, with victims facing lifelong medical bills, lost income, and emotional trauma caused by negligent care.
From surgical errors to nursing home neglect, these categories of malpractice dominate Minnesota courtrooms because they leave behind devastating consequences that ripple through patients’ lives and their families. Lawsuits in these areas are not only about recovering compensation—they serve as a powerful tool for accountability, driving systemic changes that improve safety standards for everyone.
Which Medical Specialties Face the Most Malpractice Claims?
Certain fields are more prone to malpractice lawsuits due to the nature of the care they provide, the speed at which decisions must be made, and the potentially life-altering consequences of even minor errors. In Minnesota, providers in high-stakes specialties such as surgery, obstetrics, emergency medicine, psychiatry, and primary care face heightened exposure. Understanding where the risks are greatest helps patients stay informed and empowers families to advocate for safer care.
High-Risk Specialties: Surgery, OB/GYN, and Emergency Care
Surgical mistakes, obstetric complications, and emergency room errors consistently rank among the leading causes of malpractice claims and some of the highest payouts nationwide. These areas involve high-stakes, time-sensitive decisions where a single misstep can have a permanent impact on a patient’s life.
Key malpractice risks in high-exposure specialties include:
- Surgery: Wrong-site operations, retained instruments, and negligent post-operative care
- OB/GYN: Delayed C-sections, birth injuries, and maternal hemorrhage or infection
- Emergency Care: Missed diagnoses of strokes, heart attacks, or sepsis under urgent conditions
Because these specialties demand rapid decisions under chaotic or high-pressure circumstances, the margin for error is extremely slim—and the consequences of mistakes can be catastrophic.
Malpractice Exposure in Mental Health and Psychiatry
Psychiatric malpractice claims often arise from a provider’s failure to identify, monitor, or appropriately manage suicide risk, psychosis, or dangerous side effects of medication. These cases are especially sensitive due to the vulnerability of patients and the added complexity of laws surrounding involuntary treatment and patient confidentiality.
Mental health professionals in both inpatient and outpatient settings carry a legal and ethical duty to protect patients, respond to red flags, and ensure safe treatment. When this duty is breached, the consequences can be devastating for patients and their families.
Lawsuits Against Primary Care and Internal Medicine Doctors
Even without performing surgery or handling medical emergencies, primary care doctors and internists are frequently named in malpractice suits. As the first point of contact for most patients, they play a critical role in diagnosis, early intervention, and appropriate referrals. A single oversight in this setting can allow serious conditions to progress unchecked.
Patients depend on primary care providers for early detection, errors at this stage can be particularly damaging—and legally actionable.
Click to contact our personal injury lawyers today
What You Must Prove to Win a Malpractice Claim
Winning a medical malpractice claim in Minnesota requires more than showing that something went wrong during treatment. The law demands that four specific elements be proven with evidence. Each element forms a critical part of the case—if even one is missing, the claim may not move forward. These requirements exist to ensure that only valid, well-documented cases of negligence proceed through the courts.
Existence of a Medical Duty of Care
Every malpractice case begins by proving that a doctor–patient relationship existed. This relationship creates a legal duty of care, meaning the provider is obligated to treat the patient in accordance with accepted medical standards.
In Minnesota, this duty arises once a provider formally agrees to diagnose, treat, or manage a patient’s care—whether in a hospital, clinic, nursing home, or even through a telemedicine visit. Establishing this relationship is essential, as it forms the foundation for accountability.
Breach of Accepted Medical Standards
Once a duty of care is established, you must prove that the provider breached the accepted standard of care. A breach occurs when a provider acts (or fails to act) in a way that a reasonably competent professional in the same specialty would not have under similar circumstances.
Examples of breaches include:
- Ignoring or misinterpreting abnormal lab results
- Delaying necessary diagnostic testing
- Performing surgery on the wrong site or patient
- Prescribing medications with known contraindications
This step typically requires expert testimony to demonstrate how the provider’s actions fell short compared to what other trained professionals would have done in a similar situation.
Causation Linking Negligence to the Injury
It is not enough to prove a mistake was made. You must also show that the error directly caused your injury or worsened your condition. This element, known as causation, is often the most hotly contested part of a malpractice case.
Examples of causation include:
- A delayed cancer diagnosis allowed the disease to progress to a later, less treatable stage
- A medication overdose caused permanent organ damage
- Failure to monitor anesthesia resulted in brain injury during surgery
Defense attorneys frequently argue that the harm would have occurred regardless of the mistake, this step often relies heavily on detailed medical records and expert witness testimony to support their claims.
Proof of Physical, Emotional, or Financial Damages
Finally, to succeed in a malpractice claim, you must prove that the negligence caused measurable damages. These damages can be physical, emotional, or financial—but they must be clearly documented and directly linked to the provider’s breach of duty.
Common recoverable damages in Minnesota include:
- Medical expenses for corrective or ongoing treatment
- Lost income or reduced earning capacity due to disability
- Pain and suffering related to prolonged recovery or permanent injury
- Mental distress such as anxiety, depression, or PTSD
- Loss of consortium in cases of wrongful death or catastrophic injury
The extent of these damages and their impact on your life, often determines the amount of compensation awarded.
Complete a Case Evaluation form now
What to Do If You Suspect Medical Malpractice in Minnesota
If something felt wrong during your treatment, or you experienced complications that seem unusual, it’s important to act quickly. Medical malpractice claims follow strict legal procedures in Minnesota, and your early actions can significantly impact your ability to recover compensation. Below are the most important steps patients and families should take if they suspect negligence.
Request and Preserve All Medical Records
The foundation of any malpractice case begins with securing your complete medical records. These records contain the critical details needed to evaluate what happened, identify potential errors, and build legal arguments.
Submit written requests to every facility involved in your care, including:
- Hospitals and primary care clinics
- Specialty practices and diagnostic labs
- Emergency rooms and urgent care centers
- Imaging facilities and pharmacies
Make sure your request includes:
- Treatment notes and progress reports
- Lab and imaging results
- Prescription histories
- Procedure records and timestamps
Comprehensive records allow your attorney and medical experts to pinpoint where errors may have occurred and build a strong evidentiary foundation.
Understand the Affidavit of Merit Requirement
Minnesota law requires that an affidavit of merit support every medical malpractice lawsuit. This is a signed statement from a qualified medical expert confirming that your case likely involves negligence.
Key points about the affidavit of merit:
- It must be filed within 180 days of initiating the lawsuit
- It must include a review of your records by a licensed expert in the same or similar specialty as the defendant
- It must state that the provider’s actions likely breached the standard of care and caused harm
Without this affidavit, your case may be dismissed even if the negligence seems obvious. This is a mandatory legal requirement, not a formality. Your attorney will coordinate this process to ensure it’s done correctly and on time.
Avoid Contacting the Healthcare Provider Directly
It’s natural to want answers from the provider or facility that may have harmed you, but do not contact them directly. These conversations can unintentionally damage your legal position.
Here’s why you should let your attorney handle all communication:
- Anything you say may be recorded or documented and used against you
- You could accidentally downplay your harm or admit partial fault
- Direct contact can disrupt your legal strategy or delay critical steps
Let your attorney handle all communication with the provider, hospital, or their insurance representatives. This protects your rights, preserves your evidence, and avoids costly legal missteps.
Speak with an Experienced Minnesota Medical Malpractice Lawyer
Medical malpractice cases are among the most complex areas of personal injury law. An experienced Minnesota malpractice attorney can help you understand whether your situation meets the legal standards for a claim, and guide you through every step of the process.
An attorney can:
- Evaluate whether your case meets Minnesota’s legal standards for malpractice
- Preserve medical evidence and records before they’re lost or altered
- Ensure you meet all filing deadlines, including the statute of limitations and affidavit requirements
- Coordinate medical expert reviews and build a compelling legal strategy
- Explain your rights, your options, and the potential value of your claim
If you suspect that a provider’s mistake caused your injury or contributed to a loved one’s suffering, consulting with a malpractice attorney is the most direct path to clarity, accountability, and potential compensation.
Why Medical Errors Persist in U.S. Healthcare Systems
Most medical errors are not the result of a single careless provider—they stem from deeper, systemic issues within healthcare environments. Problems such as chronic understaffing, over-reliance on automation, and weak accountability structures allow mistakes to repeat and compound. By understanding these root causes, patients and families can better recognize risks, advocate for safer care, and demand higher standards from hospitals and providers.
Understaffing and Provider Fatigue
Staffing shortages and long, demanding shifts remain one of the biggest drivers of preventable medical mistakes. Exhausted nurses, physicians, and specialists are more likely to miss subtle warning signs, misinterpret charts, or delay urgent care decisions—especially in high-pressure environments like surgery and emergency medicine.
Key risk factors linked to understaffing and fatigue include:
- Burnout: 1 in 3 nurses report burnout directly tied to staffing shortages (NIH).
- Errors: Fatigue has been linked to higher surgical complication rates and ER diagnostic mistakes.
- System strain: Short-staffed hospitals often see longer wait times, increased infections, and higher readmission rates.
When healthcare teams are overstretched, patient safety is compromised at every level.
Over-Reliance on EMRs and Automated Systems
Electronic Medical Records (EMRs) have revolutionized patient care, but they also introduce new risks when overused or poorly managed. Automation should support—not replace—critical thinking. When providers rely too heavily on templates and alerts instead of individualized assessments, serious harm can result.
Examples of EMR-related risks include:
- “Alarm fatigue,” where constant alerts are silenced or ignored
- Copy-pasted notes that miss crucial updates in patient status
- Diagnostic templates overriding unique patient symptoms
- Technical glitches that delay lab results, imaging, or medication orders
Technology should be a safeguard. When it becomes a substitute for clinical judgment, malpractice is far more likely.
Weak Internal Oversight and Reporting Mechanisms
Hospitals that lack strong internal accountability systems often repeat the same mistakes. When errors are swept under the rug or ignored, dangerous patterns take root—and patients pay the price.
Common failures in oversight include:
- No mandatory incident reporting or tracking systems
- Lack of peer review or constructive feedback after mistakes
- Leadership is failing to act on staff safety complaints
- Poor communication across departments, shifts, or facilities
These weaknesses not only endanger patients but also heighten legal liability for hospitals, especially when a preventable error occurs more than once. Strong reporting systems and responsive leadership are essential for breaking cycles of negligence.
How Common Are Medical Malpractice Claims in Minnesota?
Medical malpractice claims in Minnesota are less frequent than in some larger states, but payouts can be significant when negligence is proven. According to the 2023 National Medical Malpractice Payout Report published by NCHStats, Minnesota ranks 34th in total payout volume across the U.S.
Here’s a snapshot of Minnesota medical malpractice statistics from the most recent data available:
| Metric | Value |
|---|---|
| Total Malpractice Payouts (2023) | $18,151,000 |
| Number of Claims Paid | 63 |
| Average Payout per Claim | $288,905 |
| Minnesota’s National Rank | #34 in payout volume |
| Most Common Claim Type | Diagnostic errors |
These figures reflect only paid claims, not all filed lawsuits. Many claims settle confidentially or are dismissed before reaching trial.
Why Some Patients Wait Too Long to File a Claim
Many patients in Minnesota delay filing medical malpractice claims due to a mix of emotional hesitation and legal confusion. These delays can lead to missed deadlines, lost evidence, or even dismissal of valid cases. The sections below explain the most common reasons patients hesitate, and why it’s critical to act sooner.
Emotional Doubt, Shame, or Fear of Retaliation
It’s common for patients or their families to hesitate after a medical injury. A parent may feel guilty for trusting a provider. A senior may fear losing access to care. Some patients worry that they’ll be seen as “just suing for money” or are concerned about potential retaliation from hospital staff. These emotional blocks are real and often powerful.
But delaying legal action because of uncertainty or shame doesn’t protect anyone. It often prevents justice and allows dangerous patterns to go unchallenged. If you are unsure, a confidential conversation with an attorney can provide clarity, without commitment.
Common Legal Myths and Misconceptions
Misunderstandings about what constitutes malpractice often prevent patients from pursuing valid claims. Below are examples of common myths and the actual facts:
- Myth: You can’t sue if you signed a consent form.
- Fact: Consent forms do not excuse negligence or substandard care.
- Myth: You need a permanent injury to sue.
- Fact: Temporary injuries, if caused by negligence, can qualify.
- Myth: If you saw multiple doctors, no one is liable.
- Fact: Liability can extend to any provider who breached their duty.
- Myth: Malpractice lawsuits always take years.
- Fact: Some settle quickly, especially with strong early evidence.
- Myth: You can’t afford a lawyer.
- Fact: Many firms, including Madia Law, take malpractice cases on a contingency fee basis.
Time Limits Under Minnesota’s Statute of Limitations
Under Minnesota law, most medical malpractice claims must be filed within 4 years of the alleged negligent act. However, that window can be shorter or longer depending on your situation:
| Scenario | Filing Deadline |
|---|---|
| General medical negligence | 4 years |
| Discovery of harm after the fact | Up to 4 years from discovery (limited) |
| Minor under 18 | Extended to age 20 |
| Foreign object left in body | 1 year from discovery |
Time matters. If you wait too long, the court may bar your claim, even if the negligence was obvious. Speaking with a Minnesota medical malpractice attorney early can help preserve your rights and give you the best chance at justice.
Frequently Asked Questions About Medical Malpractice Claims
Do all medical errors qualify as malpractice?
No, not all medical errors qualify as malpractice. To qualify as malpractice, the error must involve a breach of the accepted medical standard of care, cause harm, and be proven through evidence, not just a bad or unexpected result.
What are the early signs that you might be a victim of malpractice?
Early signs of malpractice include worsening symptoms, conflicting diagnoses, sudden discharge, or care that feels rushed or dismissive. To spot malpractice early, watch for unexplained complications or providers ignoring concerns, especially after procedures or medication changes.
Can multiple errors be part of one malpractice claim?
Yes, multiple medical errors can be part of one malpractice claim. To include them, each error must contribute to the harm. For example, a misdiagnosis followed by a surgical error may combine into a single actionable case.
What should I do if I suspect I was misdiagnosed?
To act on suspected misdiagnosis, request all medical records and get a second opinion immediately. Misdiagnosis becomes malpractice if it delays proper treatment and causes harm. Consulting a medical malpractice attorney helps determine if legal action is appropriate.
Can I file a malpractice claim if symptoms got worse due to the delay?
Yes, you can file a malpractice claim if delayed care worsened your condition. To file, you must prove that the delay in treatment directly led to more serious or lasting harm than timely care would have prevented.
Still Have Questions About Medical Malpractice in Minnesota?
It’s common to have doubts after a medical setback, especially when answers are unclear. You don’t need all the facts to start asking the right questions. Determining whether your experience constitutes legal malpractice under Minnesota law begins with understanding your rights and the options available to you.
If you believe something went wrong with your care, don’t second-guess yourself. The right legal guidance can help you move forward with confidence and clarity. Contact Madia Law LLC Now!
Call 612-349-2729 or complete a Case Evaluation form